 There were concerns early in the COVID-19 pandemic that immunity to the disease caused by the SARS-CoV-2 coronavirus would be fleeting, due to the rapid decline in antibody levels documented in the months following the recovery of CODID-19 survivors. A new study out of Rockefeller University has confirmed that SARS-CoV-2 antibodies don’t linger in the body for very long, but also found that the part of the immune system responsible for remembering how to make those antibodies can do so for much longer—and may actually be able to produce improved versions of the protective molecules if faced with another infection
There were concerns early in the COVID-19 pandemic that immunity to the disease caused by the SARS-CoV-2 coronavirus would be fleeting, due to the rapid decline in antibody levels documented in the months following the recovery of CODID-19 survivors. A new study out of Rockefeller University has confirmed that SARS-CoV-2 antibodies don’t linger in the body for very long, but also found that the part of the immune system responsible for remembering how to make those antibodies can do so for much longer—and may actually be able to produce improved versions of the protective molecules if faced with another infection
The researchers studied the antibody response of 87 COVID-19 survivors at one month and six months after their respective infections, and found that the ability of the volunteers’ blood plasma samples to neutralize the virus was reduced five-fold due to a marked decrease in their antibody counts after the six month mark. However, the memory B cells (MBC), a type of white blood cell that can preserve the blueprint for a given antibody for decades, specifically the ones associated with the SARS-CoV-2 antibodies, did not decline in number, and even slightly increased their numbers in some cases.
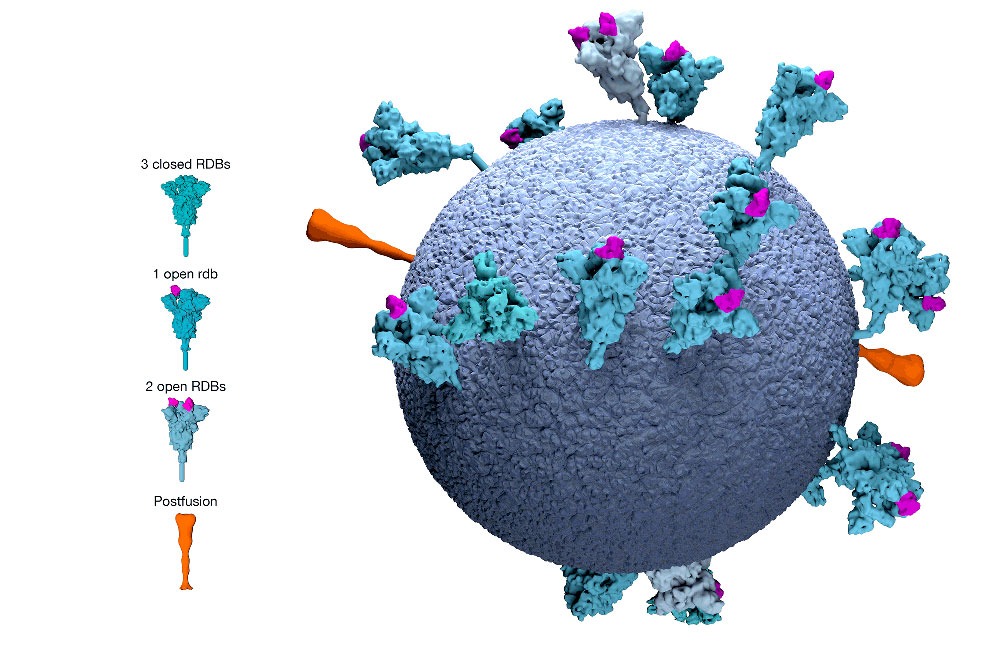
“The overall numbers of memory B cells that produced antibodies attacking the Achilles’ heel of the virus, known as the receptor-binding domain, stayed the same,” explains Christian Gaebler, a physician and immunologist with the Laboratory of Molecular Immunology. “That’s good news because those are the ones that you need if you encounter the virus again.”
The research team’s analysis also revealed that the memory B cells had gone through numerous mutations, even after the infection was resolved, and as a result the antibodies they produced were much more effective than the ones originally generated by the subjects’ immune systems.
“We were surprised to see the memory B cells had kept evolving during this time,” according to Michel C. Nussenzweig, the head of Rockefeller’s Laboratory of Molecular Immunology. “That often happens in chronic infections, like HIV or herpes, where the virus lingers in the body. But we weren’t expecting to see it with SARS-CoV-2, which is thought to leave the body after infection has resolved.”
“This is really exciting news,” says Nussenzweig. “The type of immune response we see here could potentially provide protection for quite some time, by enabling the body to mount a rapid and effective response to the virus upon re-exposure.” This promising response was found not only in patients infected with earlier strains of the virus, but also the more recent mutated strains that are causing concern amongst health officials worldwide.
The researchers suspect that this improved memory B cell function might be due to the lingering presence of SARS-CoV-2’s genetic material and its proteins in the cells that line the intestines, found in half of another group of 14 COVID-19 patients. However, the researchers aren’t sure if this is indeed the case or if the viral remnants are still infectious, or are simply the remains of dead viruses. They plan on broadening their study to determine the role the viral remnants might play in both the progression of COVID-19 and in immunity to the disease.
Subscribers, to watch the subscriber version of the video, first log in then click on Dreamland Subscriber-Only Video Podcast link.
I have a friend who had it twice. The second time was far worse than the first. How does that work?
EVIDYKS, some people who get exposed to the SARS-CoV-2 virus receive a lesser or greater total “dose” (quantity of virus) because they acquired a lesser or greater viral load … so for example, a greater exposure over a longer time to the infectious source typically results in a more severe illness.
But there are other possible factors: 1) Was your friend a recovered cancer patient, or recovered from some other illness that weakens the human immune system over time? 2) Was your friend an older person, say over age 60? Elders typically have weakening of the immune system as part of the aging process in their later decades of life.
So the answer to your question involves many complexities. More US TV news stations (and sometimes newspapers) have started featuring ‘Ask The Doctor” Q/A sessions about COVID-19. For example, in the Los Angeles, CA area, local broadcast TV news station ABC7 has frequent COVID-19 Q/A sessions with Anthony Cardillo, MD, an emergency department physician at a local hospital. And on Wednesday, January 27, 2021, at 8pm US Eastern Time, CNN cable TV will feature a 1-hour special show on COVID-19 vaccines, the virus variants, and other issues, hosted by Sanjay Gupta, MD (neurosurgeon and chief medical reporter for CNN) and Anderson Cooper, news anchor at CNN.